It is very difficult for the media to provide up-to-date information on the rapidly changing COVID-19 outbreak. What started as atypical pneumonia in Wuhan, Hubei Province, China, in December 2019 was soon revealed to be caused by a new virus, COVID-19.
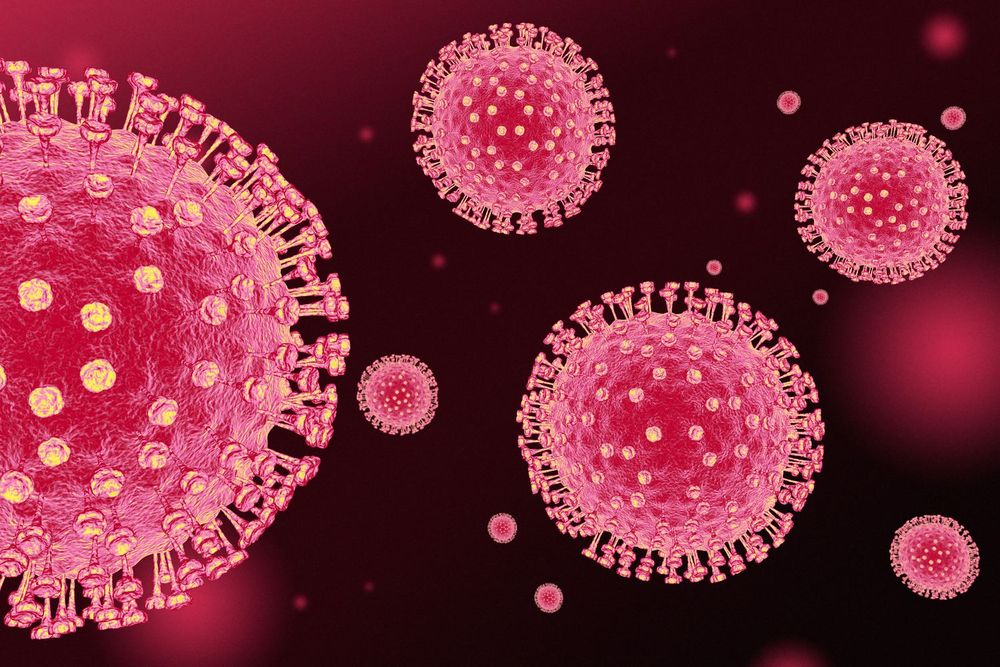
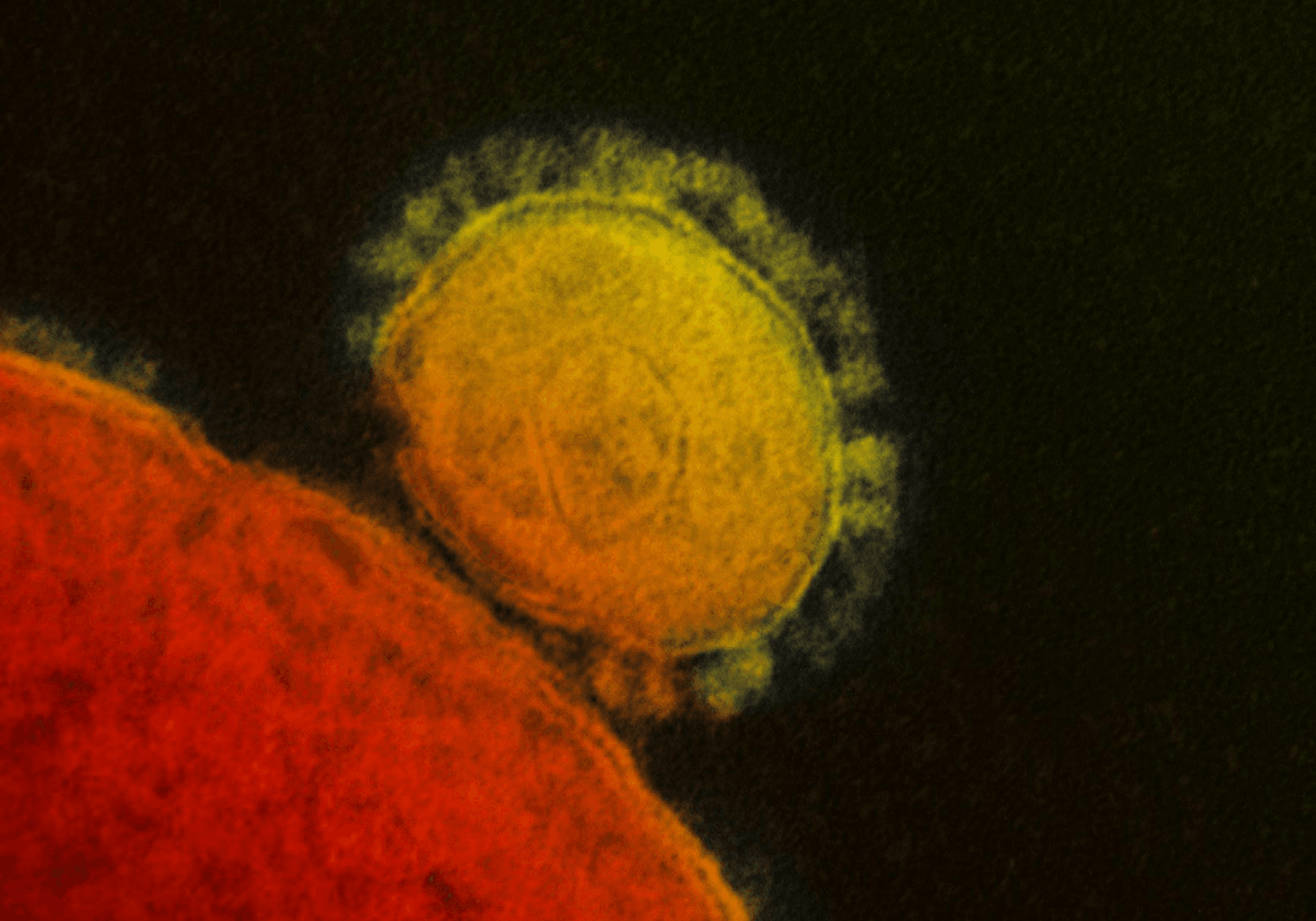
The Corona of COVID-19
In the following days, epidemiologists revealed that the disease originated in the seafood market of Wuhan. It is no coincidence that we find these types of zoonotic viruses, viruses that come from animals, in similar markets.
In these markets, different animals that are not typically eaten such as snakes, large mice, bats, and wild cats, and farm animals such as pigs and chicken are sold side by side.
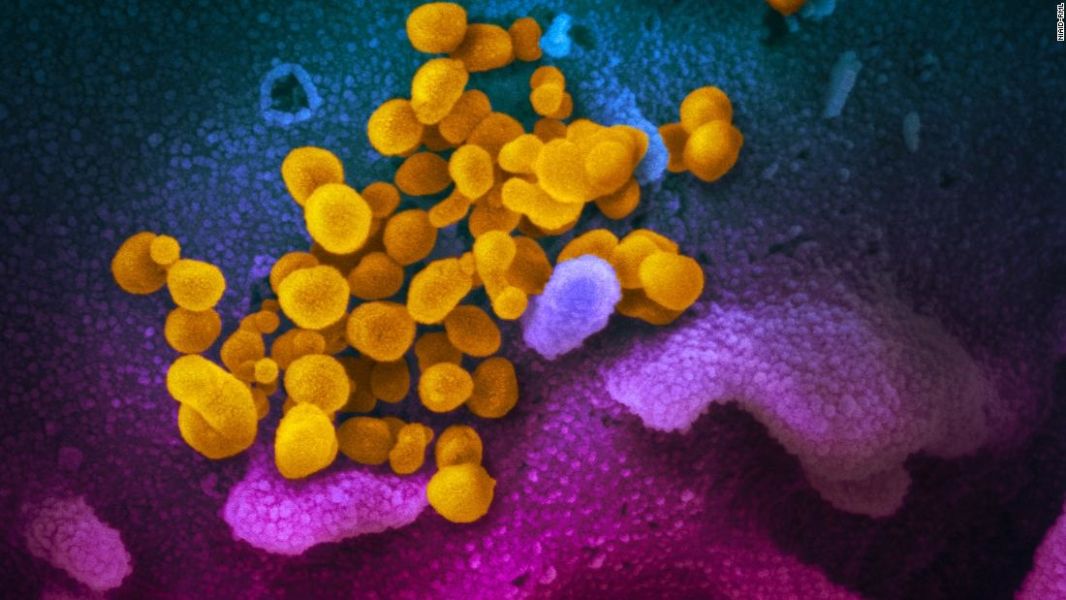
Virus Entering The Cell
What is the relationship between these sales and the outbreak of diseases such as SARS?
Viruses are protein capsules that contain either RNA or DNA. COVID-19 is a single-stranded RNA virus. The proteins in the sheath of the virus determine which cells it will enter, which means that every virus doesn't connect to every cell. Therefore, different viruses cause different diseases in different organs. For example, common cold viruses cause infections of the upper respiratory tract while COVID-19 causes infection in the lungs.
How does it make this choice?
The antigens in the protein structure can only attach to the membranes of certain cells, in this case, those of the respiratory system. Think of these proteins as keys to our cells. As soon as they attach to the cell, they can enter through the cell membrane, just like a door opening with a key. If we have the antigens that protect against the virus proteins, also known as antibodies. Then our immune system already knows this particular virus due to previous disease or vaccination. The virus cannot enter our cells. That’s why vaccinations are so important.
How come our antibodies can't stop COVID-19?
As previously mentioned, viruses don’t cause disease in every cell. Similarly, not all viruses cause illness in humans, and those that infect humans don’t necessarily infect animals.
So how does this transition work?
Some animals are susceptible to viruses that cause disease in both humans and animals. This means that they can get sick with both types of viruses.
Two viruses, only one of which can infect humans, enter the animal cell at the same time.
Which animals can affected?
Although these vary virus to virus, this situation can occur in chimpanzees, bats, pigs, and even poultry. These animals can contain both the human-infecting virus and animal-specific virus in their bodies at the same time. Both of these viruses can enter the target cells in that animal simultaneously, releasing their genetic material inside the capsules. This causes the animal to become a carrier of both pathogens.
Viruses cannot reproduce when they are not in a cell. They lie dormant, neither dead nor alive. Whether it lives or not depends on its ability to connect with a suitable host and enter its cells to replicate... On the rare occasions when both viruses release their genetic materials into the same cell at the same time, these genetic materials can mix and create a new virus that the human immune system has never seen before.
The combination of both viruses results in a new virus that can cause disease in humans.
A virus that has mutated in this way, with an antigenic drift or an antigenic shift, is now dangerous to us since we have never encountered it before. Our natural immune systems do not work against this mutant virus. We have no vaccines that will protect against it.
How contagious is this new virus? How deadly? What is its antigenic nature? What is the incubation period and what is the genomic code?
None of the answers are clear. That's why our knowledge of new viruses, including COVID-19, is constantly changing. As the number of people getting sick increases, we learn what that virus is. Something that was believed to be a simple cold turned into a deadly infection in a short period of time.
This is what we know about COVID-19 at the time of this writing:
Cause of infection: COVID-19 is a RNA virus that is contagious among humans. It is genetically similar to the SARS virus by 79.5% and to the bat coronavirus by 96%. It is believed that the virus originated in bats and later passed to humans. However, the pangolin is thought to be the transmission animal in this case.

Contagion:
Airborne transmission of the virus from person to person is possible at close range. Droplets that contain the virus can easily initiate infections from a maximum of 6 feet (1.8 m) through coughing or sneezing. For this reason, sick people should wear masks, and everyone should wash their hands thoroughly and frequently. Although not proven, it is believed that virus transmission during the incubation period is possible...
On February 1, 2020, the World Health Organization issued a statement that asymptomatic cases can also be contagious. Links between Wuhan, where the disease started, and many crowded cities of the world were an important factor in the spread of the disease before the world realized what was happening. After the outbreak was identified, 33 million people were quarantined in Wuhan and Hubei Province. This quarantine was the largest quarantine in world history to that date.
The Chinese government set up a field hospital and quarantine center for 1000 people in five days. This was an important indicator of how seriously China took this outbreak. After the genomic structure of the virus was found, this genomic code was sent to the world's leading laboratories so the search for a vaccine could begin.
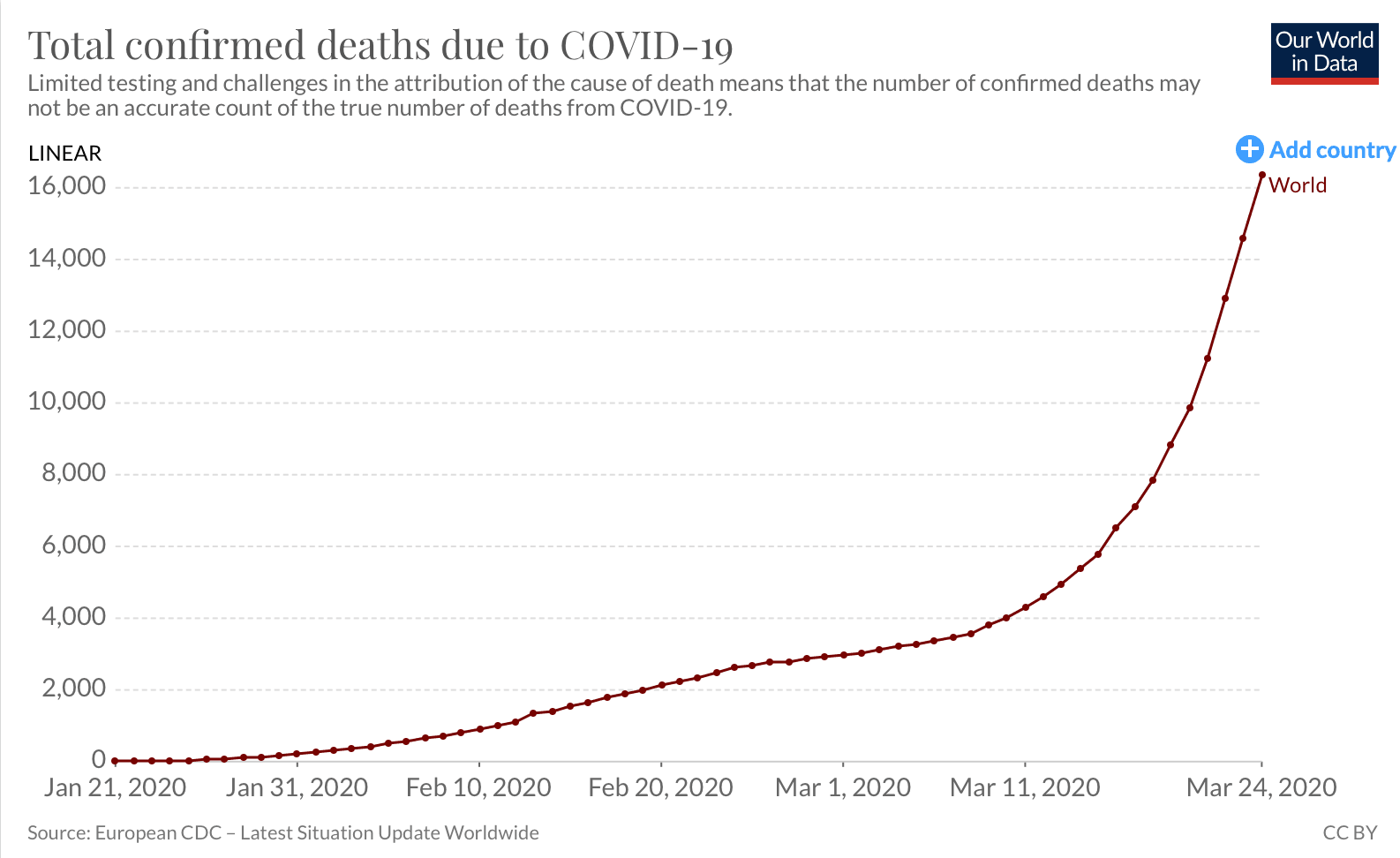
At the time of this writing (March 24, 2020), the condition of the disease is as follows:
Total number of cases: 392,255
Distribution of these cases: China: 81,171, Italy 63,927, USA 46,168, Spain 39,673, Germany 30,150, Iran 24,811,
France 19,856, Switzerland 9,117, S. Korea 9,037, UK 6,650, Austria 4,791, Netherland 4,749, Belgium 4,269, Norway 2,647,
Australia 2,136, Canada 2,091, Portugal 2,060, Sweden 2,059, Brazil 1,960, Israel 1,656, Malaysia 1,624, Denmark 1,577,
Turkey 1,529, Chechia 1,289, Japan 1,140, Ireland 1,125, ....
Number of people who died from COVID-19: 17,147
Number of people who caught COVID-19 and recovered completely: 103,389
COVID-19 Case and Death Charts
Many countries are using quarantine measures to try to reduce the spread of the disease and minimize the rate of death.
What is the mortality rate?
According to current data from the World Health Organization, the mortality rate of the virus is 2.2%.
What is the contagion rate (R0)??
The current contagion rate is 3. This is a very high rate, so protection is very important.
Source: https://www.worldometers.info/coronavirus

How long is the incubation period?
The incubation period is estimated at 2-14 days, with three days being the average. Although some studies extend this to 24 days, researchers believe that this long period is caused by secondary infections, not by infection from a primary source.
Are masks protective?
No. Wearing a non-medical face mask will not protect you from a direct cough or sneeze from an infected person. However, it can lessen the likelihood of spreading the virus by trapping the droplets when the wearer coughs or sneezes.
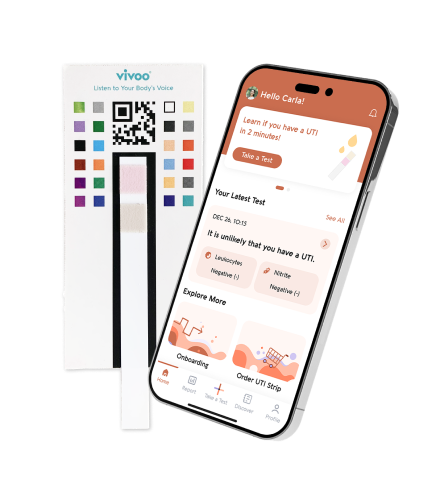
Diagnosis
The World Health Organization has published protocols for diagnosis.
What are these criteria?
Symptoms of COVID-19 include fever, shortness of breath, pneumonia spotted by tomography, and a decrease in blood values of leukocytes or lymphocytes.
It is very important whether patients with these complaints have traveled to the region where the disease originated. Or, if they have come into contact with people who recently traveled to that area. If this type of contact is suspected and the patient has symptoms of pneumonia, these individuals must be examined for the virus. A real-time RT-PCR (reverse transcription-polymerase chain reaction) test is required for blood or bronchial secretions. The results will be available anywhere from a few hours to a few days later.
Since Chinese scientists have shared the genetic sequence of COVID-19 with the world, many laboratories have been working to develop new PCR tests on this illness.
Treatment
Currently, COVID-19 has no specific forms of treatment.
Supportive treatments are being used. Oxygen support if oxygen levels are low, providing hydration, observation of fever, proper nutrition of the patient, and supporting the immune system are some of the methods.
Protection from Covid-19
The first step of protection is isolating people from risky regions for 14 days.
It is also very important to pay attention to hand-washing and the cleanness of the air we breathe as all kinds of disease agents are more intense in indoor environments and the spread of the disease becomes easier. Masks do not protect people who are not sick from the virus, but if sick people wear N95-type closed masks, they can protect those around them from infection. COVID-19 can contaminate through the air a maximum of 6 feet (1.8 m), but droplets on hard and shiny surfaces may remain highly infectious for up to 9 days.

Avoiding crowded places such as malls, schools, workplaces, and public transportation is recommended. In high-risk areas, good ventilation, frequent replacement of air filters, and disinfecting frequently touched surfaces are the most important preventive measures.
Airports, hospitals, and other healthcare institutions especially should be clean and disinfect.
The ventilation of infectious disease departments in hospitals and their separation from other parts of the hospital are also vital for preventing transmission to patients with low immune resistance. Public transportation should be properly ventilated to avoid spreading droplets through the air.
Similarly, frequently-touched surfaces at airports and on airplanes, such as armrests and tray tables, should be wiped and disinfected. In hotels, devices such as telephones and remote controls must be cleaned since they could have been touched by an infected guest. Staff should be instructed on how to properly clean hard surfaces with soap and water or other types of disinfectants.
Individuals can help protect themselves with frequent and thorough hand-washing. After going out or touching any surfaces, it is important to avoid touching the face area with unclean hands. Maintaining a distance of 6 feet (1.8 m) between people may also help slow the spread of the virus.

Developing A Vaccine and COVID-19
Vaccine production has remained largely unchanged for 70 years. The virus was obtained from infected people and isolated., then injected into chicken eggs and incubated for several weeks. The multi-stage process took months or even years and was too slow for diseases that saw daily casualties.
Fortunately, in recent years, breakthroughs have been made. In 2013, the avian influenza outbreak, known for its H7N9 antigenic structure, was the first to use new technologies. This outbreak was largely contained thanks to a vaccine that was developed much faster than its counterparts.
National Medal of Science winner Craig Venter and Nobel Prize winner Ham Smith began working on a biological printer that would read and rewrite DNA codes. They obtained information from the Human Genome Project, which aimed to unravel the entire genetic structure of a person. The important thing when making a biological printer is that it must read the genomes correctly and also rewrite the codes without errors. The editing software that orders these letters precisely and creates the desired cell was also found during these studies. The " novel application of isothermal in vitro recombination," also called the Gibson Assembly, allows codes with more than a million letters to be written without a single error.
BioXp Biological Printer
These technological developments resulted in the creation of a printer named BioXp in 2013. Thanks to this biological printer, a virus genome could send via e-mail to labs all over the world, thereby accelerating vaccine production. BioXp was printing in pieces, which process is still slow, but it was faster than before. Since BioXp’s invention, a converter that converts digital data into biological material has been made. As a result, the incoming digital data can be transformed into a biological product in a short time, thus changing the way we make vaccines completely.
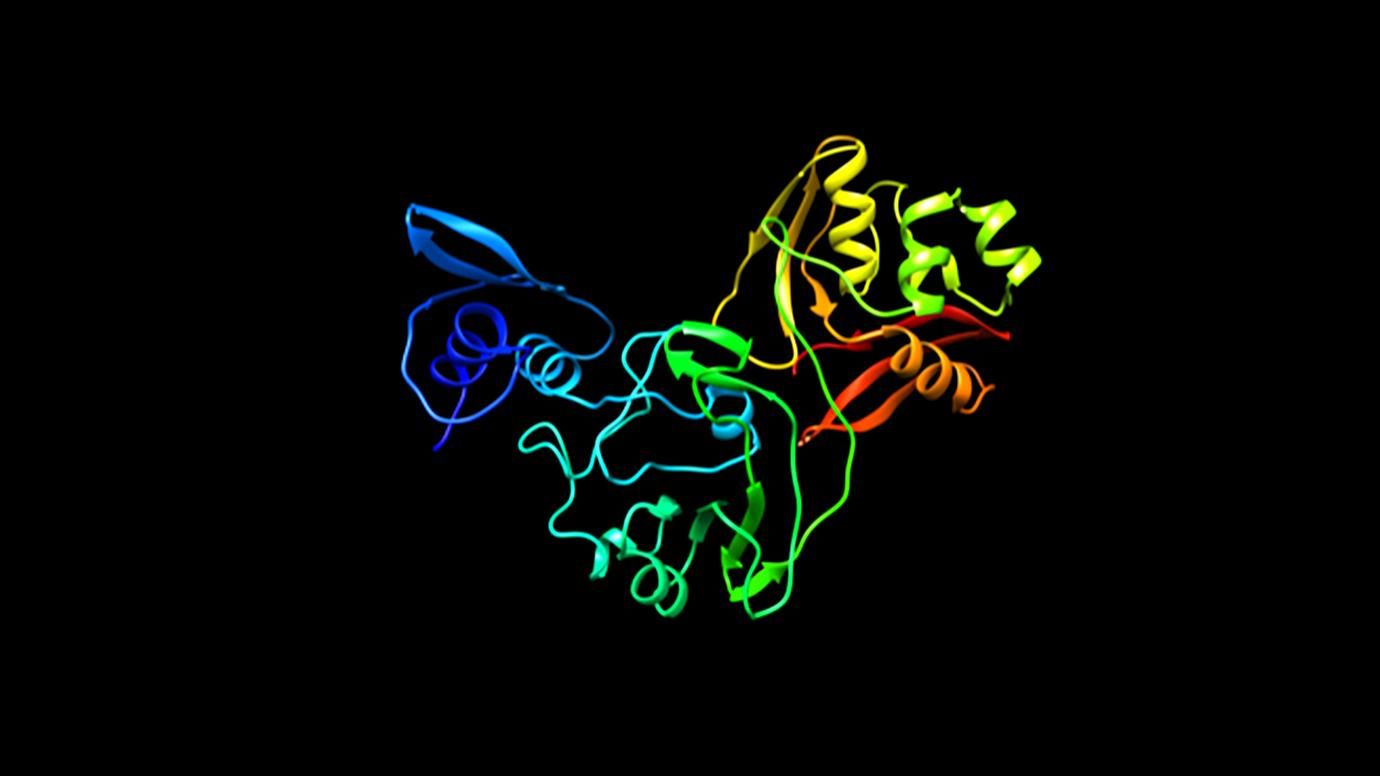
Three-dimensional modeling of proteins that provided adhesion to the virus began.
Genetic engineers, molecular biologists, mathematics specialists, and computer software and hardware engineers all started working together. 3D modeling of viral proteins and the development of appropriate drugs and antibodies were aided by artificial intelligence, allowing the duration of drug and vaccine development to shorten. Vaccine making revolutionizes with vaccines prepared faster than ever before. A report by the Reuters News Agency for the COVID-19 vaccine, based on the US National Institute of Allergy and Infectious Diseases, COVID-19 vaccine could be ready to start human experiments within three months. (https://www.reuters.com/article/us-china-health-vaccines-idUSKBN1ZN2J8 )
While there are vital developments such as the preparation of vaccines in the digital world, we are also experiencing an epidemic of misinformation that is spreading faster than ever. Not a single day goes by without new false information appearing on social media platforms. Disaster scenarios, accompanied by attention-grabbing visuals, are often shared. For example, an image of Kate Winslet, a doctor in the movie “Contagion,” shared under the title of “a deceased doctor during the COVID-19 outbreak.”
The mutation rate of COVID-19 described in the same way as the virus that destroys humanity in the movie “The Strand” by Stephen King.
Misinformation is also rampant in the forms of suggestions on how to protect yourself against the virus or where it may have come from. Rumors ranging from using hot water or salt water to clean the throat to conspiracies that the virus is a commercial attack from various countries confuses the public and increases panic. Some “experts” are also guilty of spreading misinformation, causing people to search for medicines or “cures” that may even be dangerous.
COVID-19 has disrupted the lives of people all over the world and will continue to do so for months to come. But there are some things you can do to help protect your loved ones and yourself. Wash your hands frequently and thoroughly with soap. Try to stay at home as much as possible, and practice social distancing if you must go out. Finally, get your information from a trusted source such as the World Health Organization.